 So often, we echo sentiments about “pulling yourself up by your bootstraps” and working hard for what we want in life, but there’s a reality we usually seem to miss. Frequently, the systems within which we work are not set up to actualize the dreams we strive for. All too often, our systems are constructed to prioritize profits and financial efficiency (the most “bang for your buck” regardless of quality), but those priorities directly conflict with our personal health. For example, let’s look at the American food system. According to the American Diabetes Association, diagnosed diabetes costs us $327 billion per year, and 1 in every 7 healthcare dollars is spent on treating diabetes and its complications. While the food system itself is not entirely to blame for the staggering costs of diabetes, it certainly plays a sizable part.
So often, we echo sentiments about “pulling yourself up by your bootstraps” and working hard for what we want in life, but there’s a reality we usually seem to miss. Frequently, the systems within which we work are not set up to actualize the dreams we strive for. All too often, our systems are constructed to prioritize profits and financial efficiency (the most “bang for your buck” regardless of quality), but those priorities directly conflict with our personal health. For example, let’s look at the American food system. According to the American Diabetes Association, diagnosed diabetes costs us $327 billion per year, and 1 in every 7 healthcare dollars is spent on treating diabetes and its complications. While the food system itself is not entirely to blame for the staggering costs of diabetes, it certainly plays a sizable part.
The Folly of American Food Systems
 How does one “pull themselves up by their bootstraps” when grains and sugars are cheaper than vegetables and fruits per calorie? For many low-income Americans, it becomes harder to justify spending an extra $2,000 a year to eat healthier options. Nearly 12% of Americans live in poverty, and 25% of single-parent households live in poverty. To put the 12% figure in perspective, we have a population living in poverty that is nearly double the population of New York state.
How does one “pull themselves up by their bootstraps” when grains and sugars are cheaper than vegetables and fruits per calorie? For many low-income Americans, it becomes harder to justify spending an extra $2,000 a year to eat healthier options. Nearly 12% of Americans live in poverty, and 25% of single-parent households live in poverty. To put the 12% figure in perspective, we have a population living in poverty that is nearly double the population of New York state.
In many areas of America, major chain supermarkets are not inclined to place stores within inner cities and/or low-income neighborhoods, and actively close and relocate stores already there into the suburbs or high-income neighborhoods. This phenomenon is called “Supermarket redlining” and contributes to the presence of food deserts, defined by the USDA as “parts of the country devoid of healthy food choices”. The presence of supermarket redlining and/or food deserts is directly tied to socioeconomic status, as evidenced by the fact that research done by the USDA found that areas with higher levels of poverty are more likely to be food deserts, regardless of whether it is an urban or rural community. The USDA research found that 23.5 million people (7% of the U.S. population) live in low-income areas further than a mile from a grocery store or supermarket, and that food deserts are also more likely to lack access to services such as banks, health care, transportation infrastructure, and parks/green spaces.
 When given a choice between eating nutritionally at a premium that will stretch their finances thin, or purchasing whatever food supplies the lowest-cost dietary energy, the choice becomes clear. On average, low-income household members do not meet federal recommendations for fruit, vegetable, whole grain, and low-fat dairy consumption. The disconnect between income and nutrition surely explains why low-cost, energy-dense foods that are nutrient poor are associated with lower education and incomes. Nearly 29% of Americans belong to the disgracefully-titled “lower class”, where the median income ($25,624) is within the federal poverty threshold.
When given a choice between eating nutritionally at a premium that will stretch their finances thin, or purchasing whatever food supplies the lowest-cost dietary energy, the choice becomes clear. On average, low-income household members do not meet federal recommendations for fruit, vegetable, whole grain, and low-fat dairy consumption. The disconnect between income and nutrition surely explains why low-cost, energy-dense foods that are nutrient poor are associated with lower education and incomes. Nearly 29% of Americans belong to the disgracefully-titled “lower class”, where the median income ($25,624) is within the federal poverty threshold.
The USDA publishes food plans consisting of healthy meals at four different cost levels, and the cost is calculated using national-average price estimates. To highlight how absurd our food system is, let’s look at their most affordable food plan and see how a family of four living in poverty would fare in today’s economy (See the table below).
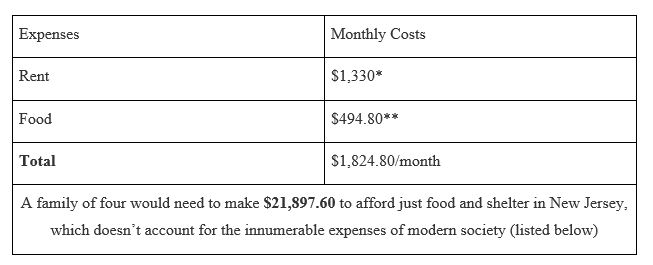
* → Source: UnitedWay of Northern New Jersey
** → Source: Official USDA Food Plans
This table does not account for ever increasing rent prices (nearly 50% of renters spend more than 30% of their income on rent, with 25% spending more than half their income on rent). This table also does not account for:
- Transportation
- Healthcare
- Childcare
- Student loans
- Phone bills
- Any “luxury purchase” such as a phone, electronics, or even clothes.
These statistics show that a significant proportion of Americans are being subjected to a food system that is actively contributing to diabetes prevalence, and goes to show how income inequality, food access and quality, and health are intrinsically linked in our landscape.
The Social Gradient & Diabetes
 Diabetes is a disease heavily influenced by diet. Both visceral fat and subcutaneous fat have been correlated with diabetes, and guess which foods have plenty of fat in them? (Answer: Cheap processed foods). Unhealthy fats (trans, saturated, etc.), sugars, meats, and processed starches increased insulin resistance, leading to higher prevalence rates of diabetes amongst those who consume those foods. Given all the information presented, one can make an educated guess as to which subsegment of the American population has more access to these foods than healthy whole foods. To nobody’s surprise, diabetes prevalence is patterned by socioeconomic status (SES), in general, but specifically within African American communities, according to an article published in the Annals of Epidemiology. The article posits that most of the risk factors associated with diabetes are also patterned by SES, meaning that your risk of developing diabetes is directly impacted by your income. The article found that even after adjusting for risk factors (behavior, diet, smoking, etc.), the association between SES and diabetes remained. The article concluded that more work needs to be done to address “underlying causes” of health disparities and why SES creates greater risks than diet or any other individual risk factor. There is even data from The National Institute for Health and Care Excellence (NICE) out of the United Kingdom that posits the same point:
Diabetes is a disease heavily influenced by diet. Both visceral fat and subcutaneous fat have been correlated with diabetes, and guess which foods have plenty of fat in them? (Answer: Cheap processed foods). Unhealthy fats (trans, saturated, etc.), sugars, meats, and processed starches increased insulin resistance, leading to higher prevalence rates of diabetes amongst those who consume those foods. Given all the information presented, one can make an educated guess as to which subsegment of the American population has more access to these foods than healthy whole foods. To nobody’s surprise, diabetes prevalence is patterned by socioeconomic status (SES), in general, but specifically within African American communities, according to an article published in the Annals of Epidemiology. The article posits that most of the risk factors associated with diabetes are also patterned by SES, meaning that your risk of developing diabetes is directly impacted by your income. The article found that even after adjusting for risk factors (behavior, diet, smoking, etc.), the association between SES and diabetes remained. The article concluded that more work needs to be done to address “underlying causes” of health disparities and why SES creates greater risks than diet or any other individual risk factor. There is even data from The National Institute for Health and Care Excellence (NICE) out of the United Kingdom that posits the same point:
“There is strong evidence for the socioeconomic patterning of the major known risk factors for type 2 diabetes in the UK i.e. for differential vulnerability. For example, obesity, central obesity, self reported physical activity, smoking, and self reported consumption of fresh fruit and vegetables are all lower in adults in the poorest compared to better off households”
Multiple studies highlight the connection between SES and urban green spaces. It’s been shown that low-income Americans are disproportionately exposed to air pollution in both the US and in areas of Europe, and that low-income Americans have less access to urban green spaces and the benefits they provide. These benefits include a decrease in all-cause and cardiovascular disease-related mortality, adverse birth outcomes, and mental disorders. This is further proof that while individual solutions can be effective and should be promoted, the societies in which we live greatly affect our health outcomes, regardless of individual behavior modification.
Potential Solutions
Most diabetes interventions focus on the individual, which is worthwhile, but is not as effective and expansive as large-scale societal interventions. Zoning regulations can be used to limit or ban fast food outlets in certain cities, restrict the number of fast food outlets in a city overall, restrict the density of fast food outlets, and regulate distance between fast food and public institutions. They can also be used to support a combination of land uses and/or Smart Growth initiatives. The construction of productive public spaces including parks, community centers, and marketplaces has a wide-ranging set of benefits. Parks provide access to green spaces and places for kids to play. Community centers provide civic programs that can boost engagement and social cohesion, and marketplaces provide a multitude of products that can benefit the health of residents.
Community gardens are a useful solution that build social cohesion, promote healthy consumption, and increase physical activity. Competitive pricing for healthy foods, as well as fruit & veggie incentive programs address affordability issues involved with healthy eating. The federal government spent more than $18 billion in 2018 on farm subsidies, with more than 31% of farmers receiving them. The products most often subsidized are corn, soybeans, wheat, cotton, and rice, which explains why rice, corn/corn-syrup and “enriched wheat flour” products are so cheap. We already pay these subsidies, so we could alter the formula to shift money around to healthier foods or create a miniscule tax to add money specifically for healthy eating. Adding nutrition education to preschool & child care curriculums creates a whole generation of children growing up with knowledge that they can impart upon their parents. School breakfast programs can be a stopgap solution for low-income children, as breakfast has been positively associated with better behavior, staying on task, and cognitive performance.
It’s imperative that we look both at the individual and at the system within the individual operates. When we see how difficult it is for many individuals to operate within that system, at what point do we stop championing personal accountability and start championing an equitable system?
Too many Americans are left to choose between healthy eating and a necessity, and almost always, the necessity takes precedence. We either need to make healthy eating more accessible, or make necessities more accessible. The worst option is to do neither and continue expecting the individual to somehow rise above insurmountable obstacles.





Join the Conversation